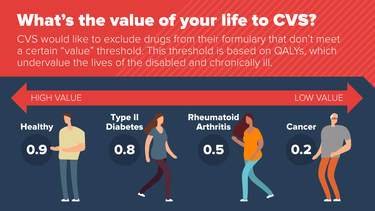
In August, CVS announced that they would offer new insurance plans that exclude drugs if they exceed a subjective “cost-effectiveness” threshold. CVS would rely on a deeply flawed value assessment model developed by the Institute for Clinical and Economic Review (ICER) in determining whether treatments fall below a $100,000 “cost per quality-adjusted-life-year” limit. This type of cost effectiveness analysis discriminates against people with disabilities and other vulnerable groups like the elderly because it assigns higher value to people in “perfect health” than people in less-than-perfect health. As the letter states, "policy decisions based on cost-effectiveness ignore important differences among patients and instead rely on a single, one-size-fits-all assessment. Further, cost-effectiveness analysis discriminates against the chronically ill, the elderly and people with disabilities, using algorithms that calculate their lives as 'worth less' than people who are younger or non-disabled."
PIPC Chairman Tony Coelho highlighted the potential implications of these cost-effectiveness thresholds in a recent blog post published in RealClearHealth. "So let’s say your child has a degenerative neurological condition and an expensive new drug is introduced that can halt, but not reverse, the damage done by the disease. Your child, and other patients like her, would be considered 'worth less' under a cost-effectiveness formula. As a result, the new treatment would not meet the threshold."
Additional information about cost-effectiveness and the concerns of patients and people with disabilities is available in PIPC's recent white paper, "Uses and Misuses of the QALY: Ethical Issues and Alternative Measures of Value."
The letter in its entirety can be read below.
| CVS Letter.pdf |
|
|
