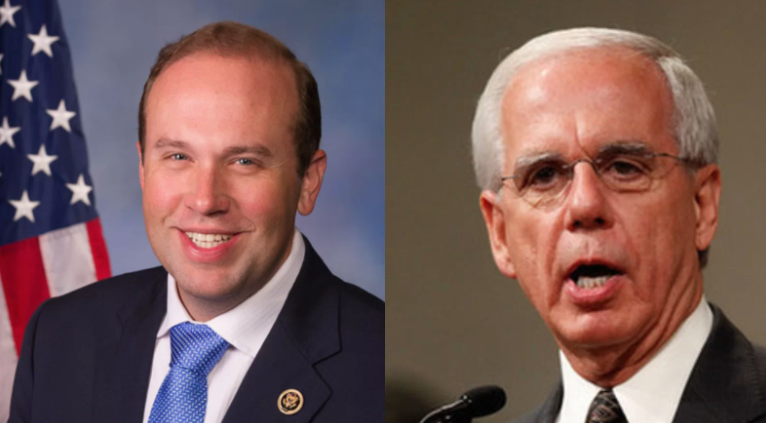
| This article originally appeared in Show-Me State Times on March 5, 2024 The U.S. House recently passed Missouri U.S. Rep. Jason Smith’s (R-8) bill to ban federal health care programs from “using prices that are based on quality-adjusted life years” (QALYs), but the chair of a national patient care group said until that bill is signed into law, a state-level bill “is needed to protect people with disabilities.” |
This op-ed originally appeared in The Hill on September 14, 2021
 This article originally appeared in Inside Health Policy on March 25, 2021 In preparation for a Senate hearing that will highlight lower foreign drug prices, a coalition that includes drug makers and patients is reminding Democrats that their 2020 party platform opposes using a metric that is key to drug-value assessments: quality-adjusted life years (QALY). 
An article for MedPage Today highlighted Partnership to Improve Patient Care's (PIPC) opposition to the Trump administration’s executive order that would import discriminatory quality-adjusted-life-years metrics into the U.S. PIPC Chairman Tony Coelho’s noted that the discriminatory metrics that the order is set to adopt would “devalue the lives of seniors, people with disabilities and serious chronic conditions." "Other countries use these metrics to ration healthcare,” said Chairman Coelho. “It is dangerous to import foreign pricing policies, and the associated access barriers that come with them."
 An article in Inside Health Policy highlighted the Partnership to Improve Patient Care (PIPC) and Value Our Health's criticism of the Institute for Clinical and Economic Review's (ICER) use of the discriminatory quality-adjusted-life-year (QALY). The article astutely points out that the QALY metric has been spurned by Congress, restricting the Patient-Centered Outcomes Research Institute's (PCORI) use of the value assessment measures. The piece also amplifies PIPC's work in pushing for value assessments that incorporate patient preferences and don't utilize a one-size-fits-all approach. "The issue we are tackling today is making sure as we move down that path, that we don’t do it in a manner that discriminates against patients,” said PIPC Executive Director Sara van Geertruyden.  An article in The Pink Sheet highlighted the Partnership to Improve Patient Care (PIPC)'s involvement with Value Our Health -- a new initiative supported by organizations representations patients and people with disabilities. The article highlights Value Our Health's opposition to the Institute for Clinical and Economic Review's (ICER) use of the quality-adjusted-life-years (QALY) metric, nothing that the patients groups have long criticized the method as a one-size-fits-all approach to addressing the needs of patients. "It is disappointing that ICER continues to reference the QALY as the 'gold standard' despite that it distorts and misrepresents how patients value their own lives, and it can lead to insurers and the government to deny care to people who would benefit from it," said PIPC executive director Sara van Geertruyden. "There are other ways of conducting value assessment, it's just they just really don't have the investment that ICER has." STAT News: ICER Says Pricing for Novartis MS Drug 'Far Out of Line,' But More Groups Push Back6/27/2019
 An article for STAT News highlighted Partnership to Improve Patient Care's (PIPC) Disability Advocate Ari Ne’eman's comments on the importance of assessing the value of medicines using treatment metrics that are specific to particular conditions or diagnosis, instead of relying on the flawed quality-adjusted-life-years (QALY) method. Ne’eman noted that due to the fact that it is inherently discriminatory against certain patients, the use of the QALY method in determining coverage for health plans is “of grave concern.” The article also amplifies Value Our Health's criticism of discriminatory value assessments during a briefing the group held, in which patient groups discussed objections to the Institute for Clinical and Economic Review’s (ICER) recent analysis of a Novartis MS drug and a new Johnson & Johnson antidepressant.  "An article for Inside Sources highlighted the Partnership to Improve Patient Care’s (PIPC) concerns regarding the Institute for Clinical and Economic Research’s (ICER) use of the quality-adjusted-life-years metric. The article amplifies comments from PIPC Executive Director Sara van Geertruyden and PIPC Disability Advocate Ari Ne’eman about ICER’s use of discriminatory value metrics in their reviews of prescription drugs, noting that these methods make patients “pawns in a profit game between Big Pharma and insurers.” “The real issue we have been trying to tackle is that it is not appropriate for patients with disabilities to be caught in the middle,” stated van Geertruyden. “Where the patient and the disability community are aligned is, their access should not be restricted as part of this path forward."  On Friday, June 14, Politico's Prescription Pulse Newsletter highlighted the Partnership to Improve Patient Care (PIPC) and over 30 patient and disability groups concerns about the Institute for Clinical and Economic Research's (ICER) 2020 Value Assessment Framework. The newsletter covers the groups' letter to ICER that criticizes its use of the quality-adjusted-life-years (QALY) metric, amplifying the coalition's message that ICER should abandon the use of discriminatory cost-effectiveness analyses. "The groups — including diabetes, epilepsy, pain and mental illness organizations — want ICER to get rid of a metric known as quality-adjusted life years that is typically used in cost-effectiveness studies to try and measure how much a therapy can improve a life," the post states. "Critics argue the measure places a lower value on the lives of people with disabilities and overestimates their burden. The coalition said it wants ICER to use models that are 'open-source, transparent, and able to generate disease-specific information.'"  In an article for Inside Health Policy, Partnership to Improve Patient Care (PIPC) Executive Director Sara van Geertruyden highlighted concerns from patient advocates about the use of comparative effectiveness data being used to limit patient access to drugs. She pointed out the problems with a "one-size-fits-all" approach, touting the Patient Centered Outcomes Research Institute's (PCORI) approached to comparative effectiveness research over the payer-focused approach taken by the Institute for Clinical and Economic Review (ICER). “Comparative effectiveness improves decision making by making sure the right patient gets the right treatment at the right time," said van Geertruyden. "But when you are talking about allowing coverage decisions based on averages to drive health care decision-making for individual patients, you allow payers and governments to drive one-size-fits-all decisions for patients." An article in STAT News notes that CVS may consider changes to its new cost-effectiveness program as a result of backlash from over 90 leading advocacy organizations representing patients, people with disabilities, physicians, and caregivers. Spearheaded by the Partnership to Improve Patient Care (PIPC), stakeholder groups criticized CVS Caremark’s decision last month to incorporate the Institute for Clinical and Economic Review’s (ICER)”quality-adjusted-life-year” metric in some of its coverage choices. “From a clinical care perspective, QALY calculations ignore important differences in individual patient’s needs and preferences,” the letter states. “From an ethical perspective, valuing individuals in ‘perfect health’ more highly than those in ‘less than perfect’ states of health, is deeply troubling.” Dr. Troyen Brennan, a CVS executive vice president and chief medical officer, responded to the letter saying that “It behooves us to spend some time to understand the concerns of the disability community and, if necessary, modify the measures so the process treats every life as being of equal value. We’ll go with the program we have now, but we’re looking for ways that we might modify it down the line.”
An article in BioPharmaDive highlights the latest pushback on efforts to establish quantitative frameworks for valuing medicines. These efforts, spearheaded by the Partnership to Improve Patient Care (PIPC), criticized CVS Caremark’s decision last month to “incorporate value-based drug pricing analyses in some of its coverage choices.” The letter, composed by many prominent groups including the American Association of People with Disabilities, the National Alliance on Mental Illness, and Vietnam Veterans of America, argues that their “main issues with ICER’s framework are not new and mirror some of the criticisms laid out by the drug industry’s trade lobby PhRMA. The article highlights that Tony Coelho, President of PIPC and former Congressman who led efforts to pass the Americans with Disabilities Act, took a strong stance on CVS’ decision characterizing it as an “outdated policy that has no place being referenced as a value-based initiative.”
|
Topics
All
Archives
July 2024
|